In 2019, cardiac surgeon and Dalhousie alum Keir Stewart (MD ’81) created the Canadian Rwanda Open-heart Project (CROP) to perform life-saving cardiac surgeries in Rwanda, with a longer-term goal to participate in the development of an independent cardiac surgery program on the base of King Faisal Hospital Rwanda.
During their last surgical mission in February this year, we engaged a few team members from the CROP team to discuss about what motivates them to come to King Faisal Hospital every quarter and what the work they do to treat patients with cardiac diseases means to them.

Myrrhisa White – Registered Nurse
I was approached last April by one of the retired nurses and one of our surgeons. They were excited to come to Rwanda to help teach cardiac surgery. For me, health equity is a very important value. So, to come to this beautiful country to help your hospital become independent is a fantastic opportunity. It is my second time here. It was definitely a refreshing and eye-opening experience to work with the Rwandan nurses, to work and learn from them and become a team together.
Each nurse has a different level of expertise and it’s really great to see them evolve. One nurse at the beginning was really shy and by the end of the mission she was hands-on and had such confidence to take care of the patients. You could see the growth personally and professionally. It is a rewarding thing to see.
Our goal here is focusing on the nurse program. We created a roadmap of the process of the patient, from their post-operative care to the time they are discharged to go home. We developed a document tool that we go through with the nurses.
A lot of the teaching happens at the bedside. From the moment the patient rolls into the room, the assessment, the different aspects of patient care and on top that, we have specialized topics we talk about including pacing, post-operative complications and we have created posters and PowerPoint presentations to go with the bedside training.
I think the success of this mission will be seeing the nurses that we are training effectively taking on the complex cases, and we’ll be standing on the sidelines watching them doing the job on their own and collaboratively interacting with the physicians. I would say we were floored by the kind of changes we found during this mission, including the new dedicated wing for Cardiovascular ICU.

Samantha Dacosta – Respiratory Therapist
The main difference between Canada and Rwanda is that we have respiratory therapists. Basically, a respiratory therapist is in charge of ventilation and that’s our job. We run blood work, we get the blood gas results, we make changes based on that, we put the tubes in and out of the mouth of the patient. I think the main difference in Rwanda is that a lot of patient duty falls on the nurses. Nurses in Rwanda and in Canada have a lot on their plate.
Additionally, my role in Canada is that I’m an educator. I work for the college there and I have students that I teach at the hospital. I really like teaching. The end goal here is that I’d love to see a respiratory therapist in Rwanda but right now the objective is to settle on having Rwandan nurses get as close as possible to respiratory therapists as they can. It’s definitely going to be a large undertaking in such a short period of time because I spent 3 years in school just learning to do that, very focused on the lungs.
I got involved in this mission because of the different roles I have been playing in Canada. My name got thrown in the hat and I was asked to come along, plus the gentleman who was a respiratory therapist during the last mission could not come. It was exciting for me as I love teaching.
In Canada we’re very lucky. Back home in Canada, we don’t have to pay for any treatment. I said if I can come here and donate my time for free for people to have these surgeries and for the staff here to learn how to take care of the patients in the future, it would be priceless for me and worth more than any paycheque I’ll ever get. My time is peanuts compared to what we’re hoping to establish at this hospital. It will be a starting point where we educate your nurse and your nurses educate others and it will trickle down to a point where you have an excellently running teaching hospital. We are just a small drop in a fountain and those ripples are going to take off and you will be able to run with it.
My experience so far is really good. I’m very hands-off when I’m teaching and with that I’m hoping to give the nurses here enough confidence to work on their own. I’m just standing right beside them observing their every step. I created an elaborate plan right from when the patient is waking up after surgery. Are they able to breathe on their own? Now that they’re ready to breathe on their own, what is the next step? Let’s do these checks. And standing there prompting and having them do everything, providing that security and having confidence in myself will enable them to have confidence in themselves as well.
It’s been great! Yesterday when we had our first patient extubated, we all had a round of applause and cheered for the team. It was wonderful! Any way I can participate as an educator is important to me. With the team of physiotherapists, we also discussed about post-operative pulmonary rehabilitation. How to have the lungs back functioning after surgery because it’s very painful for the patients after surgery.
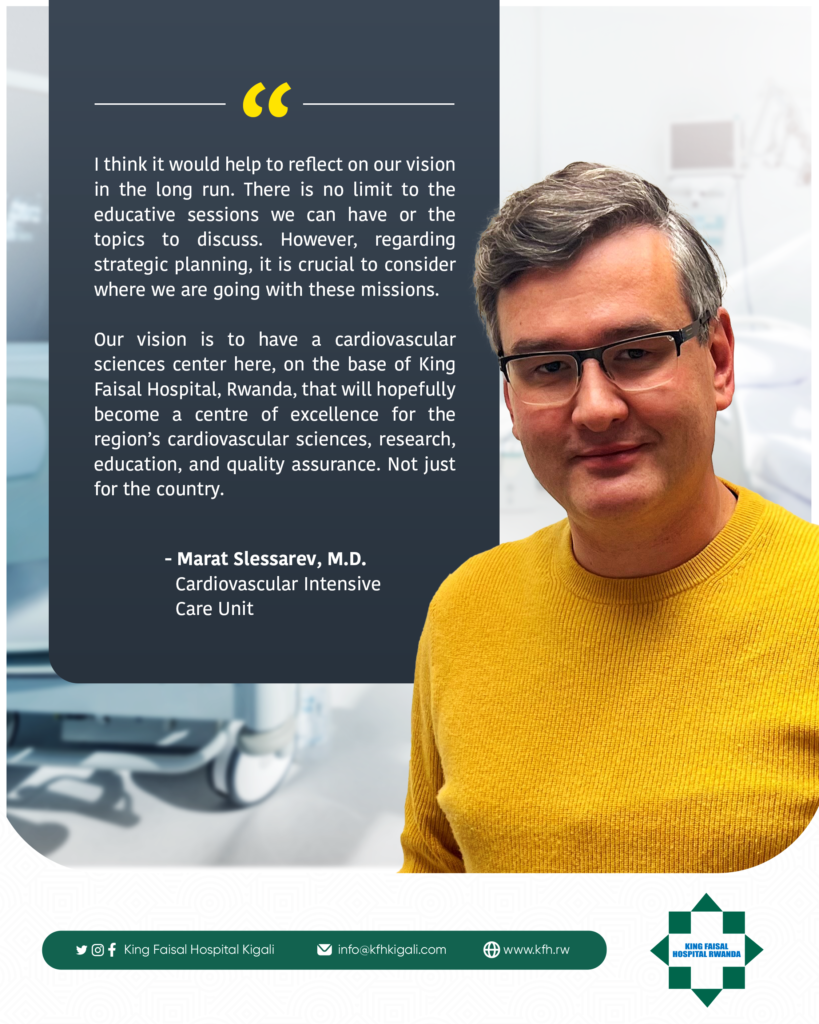
Dr. Marat Slessarev – Medical doctor- Cardiovascular Intensive Care Unit
I think it would help to reflect on our vision in the long run. There is no limit to the educative sessions we can have or the topics to discuss but in terms of strategic planning it is important to think of where we are going with these missions. Our vision is to have a cardiovascular sciences centre here, on the base of King Faisal Hospital, that will hopefully become a centre of excellence for cardiovascular sciences, research, education and quality assurance for the region. Not just for the country.
I think this is achievable and can be done through enough partnerships with universities/colleges. It takes a team. In that spirit, I’m hopeful we will not only educate providers to provide services but we will also train educators from Rwandan staff who will then take the next step to educate others across the country. The vision is to have a centre for cardiovascular sciences and then referral centres scattered across the country where educators from the hospital will be able to provide more trainings.
In terms of teaching philosophy, taking care of post-cardiac surgery patients takes a team. Any intensive care unit takes a team and that’s why we have nurses, respiratory therapists, physicians, physiotherapists, dietitians, pharmacists, etc. We have a number of experts in various fields who have to work together to take care of the patients to ensure an effective transition post-surgery.
We have to work on team dynamics and teamwork and that’s what we are trying to emphasize during this mission and future missions. One specific example is how do we run rounds? There is a dedicated time where we run around our patients, usually 2 or 3 times a day and structuring those rounds is not so much about what’s being said but rather how it’s said and organized. So, a resident physician can present a quick summary of the patient and the nurse can make an assessment from head to toe focusing on individuals and the physician can develop a plan moving forward and once those 3 people have spoken, the rest of the team can provide their inputs as well on the treatment course moving forward.
The ultimate goal is to have fellows running their own rounds at some point. I know in any institution hierarchy matters to get things running but if we are focused on working as a team, that hierarchy needs to be flattened. We have a patient; we have a mission and everybody has to contribute towards that mission. Everybody’s got a role to play and one person is not the centre of attention.
We are very aware the cases we work on are very complex, things can go wrong very quickly not because the nurses or physicians don’t know what they are doing or the patient is very sick but because emergency situations can get very overwhelming for individuals and it can become chaotic.
We have developed a training we call Crisis Resource Management and it is not only reserved for ICU care, it also happens in operating rooms, it happens in airplanes. It teaches us when we have disasters happen, what can be done right in that moment.
On Monday, we will start having low-fi simulation exercises. In-situ scenarios where we use dummies to train for emergency situations. For example, if a patient loses their pulse or have an abnormal heart rhythm, what would you do? We get team members to role-play. For example, in a certain situation if I have to use a defibrillator, where can I find it, once I find it, how will I turn it on and what mode will I use, and all that while the patient’s state is deteriorating? We try to recreate the pressure of the potential situation in a safe environment and see how people respond to it.
I can only dream that in a near future, we will have a simulation lab here, where we can use mannequins and actually do high-simulation exercises. It helps develop not only individual confidence but also confidence of working in a team. Once you have that confidence, routine stuff becomes easy because you know how well you can perform in a crisis situation.
Another part of the mission is program development. Since the cases we work on are complex, sometimes you can forget things. We have developed standardized admission notes so when the patient comes from the operating room, we have every step on where to take it from there written down. We also have a standardized order set to make sure we order the right medications, etc. With standardized processes, you move from chaos and crisis to standardization, confidence and the ability to perform on your own.
To summarize everything, The Canadian-Rwanda Open Heart Mission main three goals are team building, working inter-disciplinarily and developing teaching programs.



Leave a Reply